Unlocking Healthcare Funding: The Power of Cost Reporting and Compelling Storytelling

This letter is for the providers who know they need more resources but have been unable to secure them.
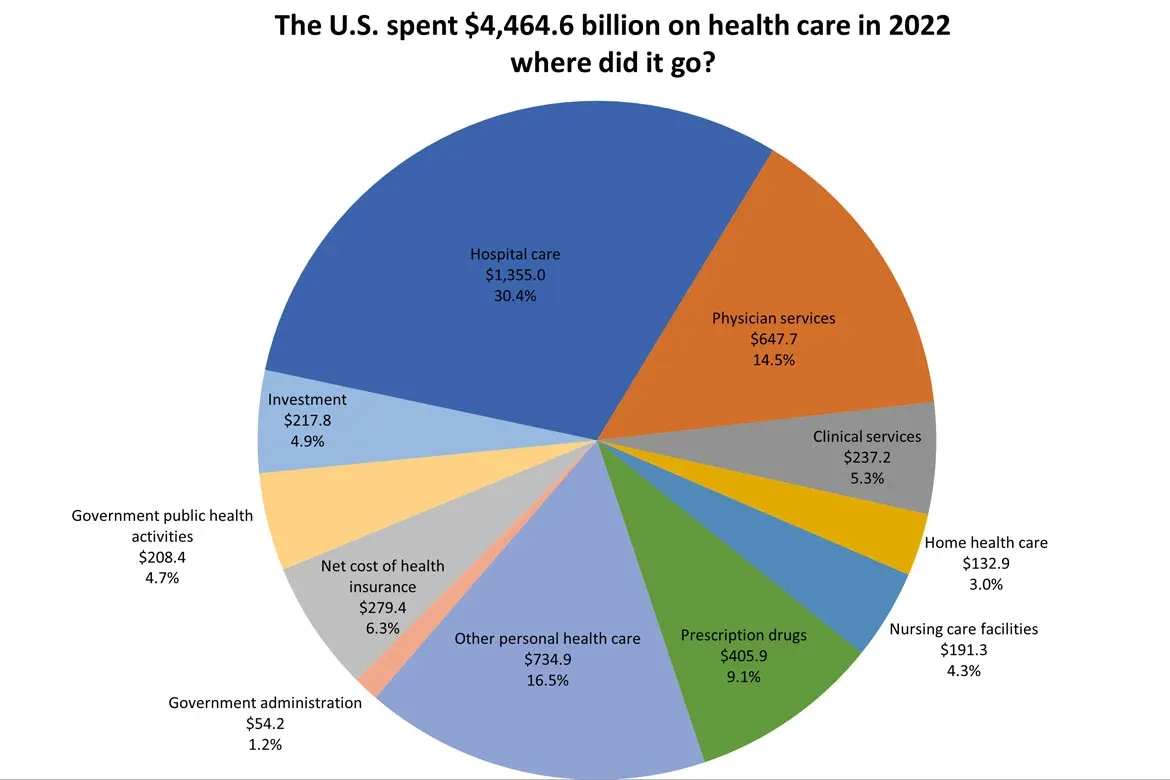
Many hospitals are facing financial difficulties. When seeking more funding, they're often accused of asking for excessive resources. As we well know, healthcare spending in the United States is one of the highest in the world.
Based on that fact alone, many believe there are more than enough resources for health care. But if you ask communities in need, there are never enough for the communities that need them. The only logical connection is, our funds are enough. But the distribution doesn't work. And that’s causing many people to lose trust in the system.
How are health systems handling this problem of insufficient funding? They are cutting services and access to patients. They are deferring the replacement of important equipment. If you can’t see this, then I’d encourage you to take part in the budget meetings of these health systems. You need to bring your thinking down to the community level instead of keeping it too macro. You can’t let a one-sided view of healthcare funding shape your mindset.
So what do we do?
- How do we get funding allocated to the communities that need it?
- How can we tell those stories in a way that persuades those who don’t believe we need more resources?
- How can we help reduce high healthcare costs without harming our hospitals?
Let’s find out.
The Funding Equation
As a health system that believes it doesn't have enough funding, how do we know when it has enough?
What are we doing with our current funding?
How do we make sense of the fact that every community would say it needs more funding?
Is adequate funding as simple as a belief? If that belief is a map to a vision, not the vision, then people will see it from many angles. They will find it far from the vision's destination.
I have a sense that we all believe that our communities can do more with more funding. We crave the opportunity to serve those needs. Many in healthcare believe in service and a greater purpose. When we don’t have that connection, we are angry, depressed, or sad in our inability to serve.
How do I reconnect to the services that matter to my community? And how do I find out what matters?
To reconnect, we must redefine the core experiences our community wants. To find what matters, we must use many views. This will help us find a way to align ourselves. We seek to fix the chaos of our current funding system.
At the base of it all, there are three general categories of health services that any community needs.
- Preventive and Primary Care
- Acute and Emergency Care
- Specialized and Supportive Care
Aligning with the highest needs
My wife accuses me of making requests that I don’t need. In effect, she is accusing me of being greedy or ineffective as a steward of the resources that I already have.
This happens whenever I can’t describe my need very well and the why associated with it. One thing is missing, though, even if I can describe the why of this request. I also need to articulate the why of every other use of funds that I am already using.
This is where I see my health systems clients fall short. They do an analysis of the need associated with a request. They articulate what it’s going to cost to provide it and they put a request together.
Yet, they forget to explain and justify the use of ALL of their costs…and it's hurting their revenue.
It's funny. Reporting costs in healthcare is fundamental. But many, including hospital CFOs and regulators, have forgotten its importance.

Much like my kids asking me for something new, the reasons why often lack clarity for the funders. The reasons that people often express are:
- I need it for my community.
- I need it or I will need to close services and reduce access.
- I need it because it’s unfair that I don’t have it.
- I need it because I’m losing money.
A decades-old process, known to all in healthcare, can fix this. It is the concept of cost reporting.
So what do I do?
When disorganized costs occur, they not only frustrate but also erode trust. Funders and stakeholders wonder if resources are being managed, even when they are. This perception can derail conversations about securing the resources your community needs.
Clear cost reporting isn’t a technical task—it’s a powerful way to shift the narrative. When you show how and why you use funds, the question shifts. It goes from, "Why should we fund you?" to "How can we help you succeed?" That shift builds trust. It ensures your community gets the support it deserves.
So how do you make your case? It starts with three steps.
Step 1: Clean Up Your Cost Groupings
The first step is getting organized. When your cost groupings are clear and consistent, you show accountability. This isn’t about appearances—it’s about showing that every dollar has a purpose.
Standardizing your reclass adjustments is a critical part of this. Errors in your numbers can hurt your credibility, no matter your needs. Accuracy is non-negotiable.
Step 2: Document the “Why” at the Cost Center Level
Once you organize your costs, it’s time to dig deeper. Why does each cost exist? How does it contribute to the outcomes your community values most?
A vague justification—“We need this for the community”—isn’t enough. Funders want to see specifics. They must see how each dollar supports the care and services your community needs.
By linking costs to outcomes, you show the need for funding. When you tie every dollar to a meaningful purpose, your case becomes much harder to dismiss.
Step 3: Tell the Story of the Year
Data is essential, but numbers alone don’t persuade. You need to weave your data into a compelling story.
What did you achieve with the funding you already had? Who benefited? What gaps remain? This isn’t about spreadsheets—it’s about showing impact. A good story changes your request for "more money" into an investment in results.
When you can show the value of your work, funders see their chance to make a difference.
Shifting the Conversation
When you master these three steps, something remarkable happens: the conversation changes. Funders stop questioning your credibility and start looking for ways to collaborate.
Instead of hearing, “Why should we give you more?” you’ll hear, “What can we do to help you achieve your goals?” That’s the power of trust, transparency, and a clear narrative.
The disconnect in healthcare funding won’t fix itself. If we want to create a system that works for everyone, we have to show that every dollar counts.
Clear cost reporting isn’t an administrative process—it’s transformational. It builds trust, strengthens relationships, and turns scarcity into opportunity.